Download the Felix App
Earn reward, visit our shop and get exclusive offers on the app
Download nowEarn reward, visit our shop and get exclusive offers on the app
Download nowPut your health first in 2026 with free visits on all categories, and $200 off longevity testing.
Download nowPut your health first in 2026 with free visits on all categories, and $200 off longevity testing.
Download now
AI-generated summaries may be inaccurate and do not constitute medical advice. Third-party AI tools are not under Felix's control, and your use of them is at your own risk.
In the early days of birth control, the pill's side effects and other forms of hormonal birth control could vary from moderate to severe. As medical and pharmaceutical research has become more advanced, birth control pills have become safer and more widely available to Canadians.
Of course, even modern-day birth control is not without side effects — and if you plan to start a prescription, being aware of these side effects is essential. By speaking with a healthcare practitioner, you can cover all the potential side effects, risk factors, and benefits of birth control pills to determine the best option for you and your body.
This article discusses the potential side effects of birth control, including which are considered typical and which may cause concern.
Keep reading to learn more about what you can expect from a birth control prescription.
Birth control is a term used to describe various methods of contraception that help prevent pregnancy. Depending on the type of birth control, it may also come with extra advantages, such as menstrual cycle regulation or STI prevention.
Though there are many different forms of birth control, they all fall into one of two main categories:
Although several birth control methods — such as birth control pills and intrauterine contraception (IUC) — are highly effective, no form of birth control is 100% effective.
In many cases, a healthcare practitioner may recommend a non-hormonal form of birth control for use in tandem with a hormonal form of birth control. For example, while birth control pills protect against pregnancy, only condoms can prevent the spread of STIs. Thus, condoms are often used alongside birth control pills.
Even then, condoms are not 100% effective at STI prevention either. This makes transparent, open, and honest communication between you are your partner(s) a necessity before engaging in sexual activity of any kind.
Within the categories of hormonal and, non-hormonal birth control are several different birth control methods for you to choose from.
Discuss your options, risk factors, and health goals thoroughly with your healthcare practitioner when choosing a birth control method. This will help your practitioner to determine the best possible method for you and your body.
Hormonal birth control is a type of contraception that uses hormones to prevent ovulation and inhibit sperm from reaching and fertilizing an egg.
Though hormonal birth control is generally considered safe for many people, some risk factors make certain types of hormonal birth control that contain estrogen unsuitable for certain patients. These patients include :
Keeping this in mind, let’s examine the main types of hormonal birth control you can choose from:
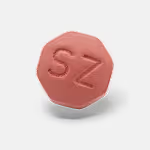
Birth control pills — also called oral contraceptives — are taken daily by mouth and contain the hormones estrogen and progestin. Some birth control pills designed for people who cannot take estrogen contain only progestin.
While birth control pills reduce the risk of pregnancy by stopping ovulation, people can also use them to help manage and regulate a person’s menstrual cycle. Additional uses for birth control can include treatment of PMS symptoms, reduced severity of menstrual cramps and flow, and endometriosis management.
There are two types of birth control pills — combination pills (which contain estrogen and progestin) and the mini-pill (which only contains progestin). As discussed above, estrogen-containing pills are unsuitable for people with certain risk factors. The mini-pill is a safe alternative that offers the same effectiveness as combination pills.
When starting birth control, several mild side effects may occur in the first one to two months of use. These side effects include:
If these side effects persist longer than a couple of months or if they worsen in severity, speak with your healthcare practitioner as soon as possible.
Rarer side effects can occur from taking birth control pills that require medical attention. You should contact your healthcare practitioner immediately if you notice any of these.
These rare side effects include:
If you are experiencing any of the above serious side effects, seek immediate medical attention.
Always speak honestly and openly with your healthcare practitioner about your medical history and lifestyle habits before beginning birth control. This will help your practitioner determine whether you have any pre-existing risk factors that may result in rare and more serious side effects.
Intrauterine contraception (IUC) — sometimes called an intrauterine device (IUD) — is a T-shaped device that is medically inserted into the uterus by a healthcare practitioner.
These devices can be both hormonal and non-hormonal, with the hormonal version releasing the hormone levonorgestrel into the uterus. IUCs can be left in place for between 3 to 10 years and are considered one of the most effective forms of birth control.
An IUC has many advantages, including being suitable for those who cannot take estrogen or breastfeed. Additionally, the IUC can help to reduce the risk of endometrial cancer.
Side effects of the hormonal IUC can include:
As for the side effects of the non-hormonal IUC, the main side effect you may experience is irregular bleeding or spotting, as well as pain or discomfort during insertion.
Like birth control pills, these side effects should subside around one to two months after the IUC is inserted. There is also a rare risk associated with IUC insertion that can result in infection and/or perforation of the uterus.
If you experience persistent or worsening side effects, contact and visit your healthcare practitioner immediately.
Birth control pills and IUCs are generally considered the most effective forms of birth control.
However, there are several alternatives for you to choose from as well. These include:
As with birth control pills and IUCs, the side effects of these alternative forms of hormonal birth control should subside on their own after one to two months of consistent use.
If side effects persist or worsen, or if you experience moderate to severe symptoms you expect may be related to your birth control method, contact your healthcare practitioner immediately.
Non-hormonal birth control refers to various methods that do not use or administer hormones to the body. While most of these methods are barrier contraceptive methods — a type of birth control that creates a barrier that prevents sperm from entering the uterus — there are also a few non-barrier methods (such as non-hormonal IUCs and surgical sterilization procedures).
The non-hormonal birth control options can often be a good alternative for those who cannot or do not want to take hormonal birth control. Additionally, certain types of non-hormonal birth control (specifically, condoms) offer the added benefit of STI protection.
With this in mind, let’s take a look at the non-hormonal birth control methods and their potential side effects:
Condoms are a barrier method of contraception made from latex or polyurethane materials. They come in both male and female versions, though male condoms are much more widely available.
Male condoms are worn on an erect penis, while female condoms are fitted inside the vagina before sexual intercourse occurs.
In general, there are no side effects related to condoms, and this method of birth control is considered widely safe due to condoms not containing active ingredients. However, if you are allergic to the materials condoms are made from, you may experience an allergic reaction.
Mild symptoms include of an allergic reaction include:
A severe allergic reaction may occur in rare cases, requiring immediate medical attention. The symptoms of severe allergic reactions include:
If you or your partner experience any of the above symptoms seek medical attention immediately.
Cervical caps are small, thimble-shaped devices made from silicone inserted into the vagina and block the passageway into the cervix. These devices can be inserted into the vagina up to two hours before sexual intercourse occurs.
When using a cervical cap, you should also use a spermicide gel. Without the gel, the effectiveness of a cervical cap can drop significantly.
For each time sexual intercourse occurs after the initial two hours have passed, you should reapply the spermicide gel to the cervical cap.
The main side effect associated with cervical caps is vaginal discomfort during use.
However, cervical caps can also present additional risk factors, such as:
If you experience symptoms of any of these conditions, seek medical attention immediately.
Sponges and diaphragms are types of barrier contraception that are no longer widely used due to their low effectiveness and potential for incorrect use. Both are inserted into the vagina and require the use of a spermicide to be effective. Even with the use of spermicide, the failure rate can be high.
Like the other barrier methods, there is potential for an allergic reaction to these devices' materials. This can include side effects such as skin irritation, hives, runny nose, or rash.
More severe side effects of an allergic reaction — such as difficulty breathing, dizziness, or confusion — require immediate medical attention.
If a sponge or diaphragm is left in too long, there is a heightened risk of toxic shock syndrome, which requires immediate medical attention.
Emergency contraception is a type of contraception used when the risk of pregnancy is heightened after sexual intercourse due to the following:
If you require emergency contraception in Canada, you have two options to choose from:
Non-hormonal birth control methods will always have lesser side effects than hormonal methods, as they do not contain active ingredients that affect the body’s chemistry.
Overall, the non-hormonal IUC offers the least amount of side effects while still providing a high level of effectiveness. Hormonal IUCs and birth control pills can have mild side effects but are generally considered safe for most people, with estrogen-free alternatives available for people who cannot take estrogen.
There’s a whole world of information about birth control and which method is best — which can often include misinformation or misleading statements.
The best way to find the proper birth control for you is to speak with a healthcare practitioner. After an honest and open conversation about your medical history, risk factors, lifestyle habits, and health goals, a healthcare practitioner can help determine your body's best birth control method.
If you are concerned about potential side effects, ask your practitioner about what side effects may occur with different types of birth control during your appointment.
To begin your birth control journey, speak with a Felix healthcare practitioner about your options today.
Medically reviewed by
References