Download the Felix App
Earn reward, visit our shop and get exclusive offers on the app
Download nowEarn reward, visit our shop and get exclusive offers on the app
Download nowPut your health first in 2026 with free visits on all categories, and $200 off longevity testing.
Download nowPut your health first in 2026 with free visits on all categories, and $200 off longevity testing.
Download now
AI-generated summaries may be inaccurate and do not constitute medical advice. Third-party AI tools are not under Felix's control, and your use of them is at your own risk.
This article discusses the safety of birth control pills for women 40 or over and the relationship between age and birth control.
Keep reading about key health risks to consider and discuss with your healthcare practitioner.
In the early days of birth control, many birth control pills contained very high doses of estrogen and other hormones that made these prescriptions risky for women over 40.
Nowadays, most birth control pills are made with a lower dose of hormones. In addition to standard birth control pills containing lower hormone levels, there are also specific types of pills that contain low doses of estrogen (10mg or less) or no estrogen at all.
As a result, it is less risky for women to continue taking birth control pills after age 40.
The key is to maintain regular communication with a healthcare practitioner about your health conditions, both pre-existing and newly developed, as well as any risky lifestyle habits you have (such as smoking).
The age at which people start taking birth control pills is highly varied, with some girls as young as 11 starting prescriptions for purposes outside of contraception, such as menstrual regulation and management.
In one study, roughly 30% of women in Canada aged 15 to 49 took oral contraceptives. The average age of the birth control users surveyed in this study was 26. For women aged 40 to 49, the percentage of birth control users dropped to just 3%.
Many pediatric healthcare practitioners will begin discussing the importance of sexual health with parents when a child reaches pre-teen years. Birth control pills are not recommended if a child has not yet started their period.
However, if a pre-teen or teen girl is experiencing painful or unwanted menstrual symptoms — or if they are open about being sexually active — a healthcare practitioner may present birth control pills as an option to parents.
Pap smears — a procedure that tests for cervical cancer — are not generally administered for women until they reach age 25, as the risk for cervical cancer is thought to be very low in teens.
If a teen is on a birth control pill prescription and has a family history of cervical cancer, then a healthcare practitioner may suggest that an annual Pap smear be performed.
Healthcare practitioners begin paying closer attention to risk factors associated with birth control pills once a woman reaches the age of 35.
This is because women 35 and older are at a higher risk for strokes, high blood pressure, and other heart-related problems.
The Heart and Stroke Foundation of Canada states that this risk is heightened if a woman over 35 also smokes, experiences migraines with aura, already has high blood pressure or has pre-existing heart-related risk factors (such as a family history of heart attacks or diabetes).
As such, women should begin discussing potential risks associated with birth control pills once they reach the age of 35. However, this does not automatically mean that a woman must stop taking birth control between the ages of 35 and 40 — it just means they must pay closer attention to certain risk factors.
Once a woman reaches the age of 40, her chances of becoming pregnant are reduced significantly.
For women who are 40, the chance of conception is estimated to be 5% each menstrual cycle.
Additionally, due to the reduced quality of the eggs released from the ovaries, pregnancies in women in their 40s are at higher risk for miscarriage or congenital disabilities.
As mentioned, certain health-related risk factors can heighten the risk of taking birth control after a woman reaches the age of 40.
These health risk factors include:
High blood pressure (hypertension) is when a person’s blood pressure in their arteries stays consistently high. Blood pressure is determined via two measurements — systolic pressure and diastolic pressure.
Systolic pressure refers to the pressure occurring as your heart contracts, while diastolic pressure occurs as your heart relaxes.
In Canada, hypertension is defined as:
The chance of high blood pressure occurring increases in women aged 35 or older. Additionally, research suggests that birth control pills with high doses of estrogen also heighten the risk of high blood pressure.
Thus, if you are 35+ years old and currently experiencing or are at risk of hypertension, you should generally avoid estrogen-containing birth control pills.
Blood clots occur naturally in the body when injuries occur to prevent blood loss.
However, blood clots can also occur in excess in the veins, travelling to the brain or lungs and causing blockages in the arteries that may result in a stroke or heart attack.
Hormonal birth control is associated with forming leg and lung blood clots, though this occurrence is rare. Nonetheless, since women 35 and older are at a greater risk for heart-related problems, it is key to consider the added risk birth control may pose in terms of blood clots.
Diabetes Canada states that people 40 or older are at a greater risk of developing type 2 diabetes.
The following factors heighten this risk:
Since estrogen-containing birth control is associated with an increased risk of developing high blood pressure, it may also contribute to your risk of developing type 2 diabetes.
Anyone over the age of 40 is recommended to get tested for diabetes once every three years. Testing should occur more frequently for anyone with one or more risk factors (besides age).
Though the risk is considered minimal, hormonal birth control pills are not recommended for women who currently have, have a history of, or have risk factors for breast cancer. Smoking women are at a higher risk for heart-related problems like heart disease and stroke.
Women over 40 who are taking estrogen-containing birth control pills should have their health regularly assessed by a healthcare practitioner. Providing as thorough information as possible regarding family history with these health conditions is also crucial.
Estrogen-containing birth control pills for women 40 years or older may not be the best option due to potential health complications.
However, several alternatives methods of both hormonal birth control and non-hormonal birth control are available, including:
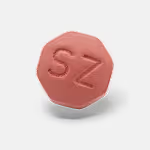
The mini-pill is a type of birth control pill that only contains progestin, a synthetic form of progesterone. These birth control pills do not contain any estrogen.
As far as the effectiveness of the mini-pill, it is considered equally as effective as estrogen-containing birth control pills at 92% with typical use and 99.7% with perfect use.
Most of these pills come in packs of 28 and do not contain any placebo pills. They are intended to be taken continuously rather than taking a 7-day hormone-free break.
However, there is a new progesterone-only pill that includes four inactive pills per pack, providing a 4-day hormone-free break.
Along with being well-suited for women 40 years or older, the mini-pill is also a good option for women who smoke, have heart-related risk factors, or are breastfeeding.
Hormonal rings and patches are a type of birth control worn for days or weeks at a time and slowly release a low dose of hormones into the body. Patches and rings contain both estrogen and progestin.
Patches are re-applied to the skin every week for three weeks straight, followed by one week with no patch. This patchless week allows for a regular period to occur.
Rings are self-inserted into the vagina and worn for three weeks before being removed on the fourth week. This fourth week allows for a regular period, after which you can insert a new ring.
Since these methods contain estrogen, you should consult your healthcare practitioner before using rings or patches if you are over 40.
While hormonal birth control methods are generally considered the most effective forms of birth control, several non-hormonal methods are available in Canada.
These include:
Tubal ligation — commonly referred to as having your “tubes tied” — is a surgical procedure in which the fallopian tubes are closed.
This surgery prevents pregnancy permanently, though it is not 100% effective. In some rare cases, women may experience a regrowth of their fallopian tubes one year after the surgery, allowing for a pregnancy. This happens to roughly 5 out of every 1,000 women.
Generally, the use of estrogen-containing birth control pills is not recommended for women over the age of 50. However, progestin-only pills can still be taken by women 50 years or older.
Additionally, women 50 years or older are highly likely to begin the transition into menopause (menopause is the end of a woman’s menstrual cycle, after which she can no longer get pregnant). For most women, menopause occurs between the ages of 45 to 55.
Once menopause occurs, and a menstrual cycle ends, there is no longer a need for birth control pills. However, barrier methods like condoms are still recommended for women who are sexually active to help protect against STDs.
Perimenopause is the transitional period that occurs before menopause.
Although you can still become pregnant and have a period during perimenopause, it is doubtful. During this transitional phase, the ovaries begin to stop working naturally. Once 12 months have passed with no period, you may be diagnosed with menopause.
Symptoms of perimenopause include:
Low-dose estrogen-containing or progestin-only birth control pills may help manage the symptoms of perimenopause and prevent pregnancy during this phase.
If you are 40 years or older and trying to decide whether or not birth control pills are right for you, talk with a healthcare practitioner.
Your practitioner can help you determine if you have any notable risk factors and which birth control method is the best option for your needs and health goals.
Get started with Felix today to discuss what birth control options may suit you.
Medically reviewed by
References